Managing Cancer-Related Pain: Interventional Radiology Solutions for Palliative Care
Cancer, a disease characterized by abnormal cell growth, is a leading cause of morbidity and mortality worldwide. As cancer progresses, patients often experience significant pain, which can greatly affect their quality of life.
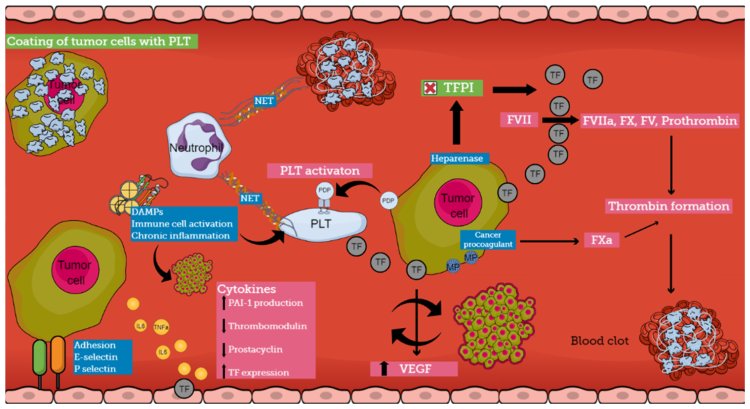
Cancer, a disease characterized by abnormal cell growth, is a leading cause of morbidity and mortality worldwide. As cancer progresses, patients often experience significant pain, which can greatly affect their quality of life. Pain associated with cancer is a complex issue, as it can arise from the cancer itself, from treatments like chemotherapy and radiation, or from other complications such as infections or blood clots.
While cancer treatment focuses on managing the disease, addressing cancer-related pain is an essential component of patient care. For many patients, especially those in advanced stages of cancer, palliative care becomes an important aspect of the treatment plan. Palliative care aims to relieve pain and other symptoms, improve quality of life, and offer support to both patients and their families.
One of the most effective and minimally invasive approaches to managing cancer-related pain is through the use of interventional radiology (IR). Interventional radiology uses imaging guidance, such as X-ray, ultrasound, or CT scans, to perform minimally invasive procedures that target the source of pain, offering long-term relief with minimal side effects and recovery time. This article explores how interventional radiology plays a crucial role in managing cancer-related pain, particularly in palliative care, and the different techniques that can be employed.
Understanding Cancer-Related Pain
Cancer-related pain is often classified into two types: somatic and visceral.
-
Somatic Pain: This type of pain occurs when cancer affects the body’s tissues, including the skin, muscles, bones, and joints. It is typically sharp, localized, and aggravated by movement.
-
Visceral Pain: This type is caused by cancer invading organs or other soft tissues, such as the liver, lungs, or gastrointestinal tract. It is often described as dull, aching, or cramping pain and can be harder to pinpoint due to the diffuse nature of the pain.
Pain may also arise from neuropathic causes, such as nerve compression due to tumor growth or from the side effects of cancer treatments. Referred pain, which occurs when pain is felt in an area distant from the site of the tumor, is another phenomenon that complicates the management of cancer-related pain.
Cancer-related pain can be persistent or intermittent, and it may worsen over time as the disease progresses. Effective management of cancer pain is a crucial aspect of palliative care to ensure that patients maintain the best possible quality of life.
The Role of Interventional Radiology in Cancer Pain Management
Interventional radiology (IR) provides a range of treatment options for managing cancer-related pain. These procedures involve the use of imaging techniques to guide a physician in performing minimally invasive interventions that target the root cause of pain. IR treatments are particularly beneficial for patients with cancer pain that is unresponsive to traditional pain medications or for those who may not be candidates for surgery.
Here are some of the key interventional radiology techniques used in the management of cancer-related pain:
1. Percutaneous Image-Guided Biopsy
Before discussing treatment options, it's important to note that pain in cancer patients is sometimes due to tumors that are not immediately identifiable. Percutaneous image-guided biopsy is a technique used to obtain tissue samples from tumors to confirm their nature and determine the most appropriate treatment. By precisely targeting tumor tissue using imaging modalities such as CT or ultrasound, this technique minimizes tissue trauma and recovery time. In cases where cancer-related pain is poorly understood or localized, a biopsy helps in diagnosing and managing pain more effectively.
2. Tumor Ablation Techniques
Tumor ablation refers to a set of procedures designed to destroy cancerous tumors without the need for surgical excision. The goal of these techniques is to shrink tumors that are causing pain, bleeding, or obstruction. Several types of tumor ablation techniques are commonly used in interventional radiology, including:
a. Radiofrequency Ablation (RFA) or Microwave Ablation (MWA)
Ablation is one of the most common methods used to treat cancer-related pain caused by solid tumors. In this procedure, a catheter with an electrode at the tip is inserted through the skin and guided into the tumor under imaging guidance, typically with ultrasound or CT scans. The electrode is then used to generate heat that destroys the tumor tissue.
-
Indications: Ablation is commonly used for treating tumors in the liver, kidneys, lungs, and bones. It is particularly effective in treating small to medium-sized tumors that are difficult to treat surgically.
-
Benefits: Ablation is minimally invasive, involves no incision, and offers relatively quick recovery. It can provide immediate relief of pain by shrinking the tumor and decreasing pressure on surrounding structures.
-
Outcome: The procedure may need to be repeated in some cases, especially if the tumor is large or the tumor regrows.
b. Cryoablation
Cryoablation uses extreme cold, rather than heat, to destroy cancerous tissue. A cryoprobe is inserted into the tumor, and a cryogenic fluid is passed through it to freeze the tumor cells.
-
Indications: Cryoablation is often used for cancers in the liver, kidney, and lung.
-
Benefits: Cryoablation is particularly useful when tumors are located near sensitive structures, such as blood vessels or bile ducts, where heat might cause collateral damage.
-
Outcome: Like RFA, cryoablation provides effective pain relief and tumor control, with minimal recovery time.
3. Nerve Blocks and Neurolysis
In cases where pain is caused by nerve compression or invasion by tumors, nerve blocks or neurolysis can be used to block pain transmission or reduce nerve sensitivity. These procedures are particularly helpful for managing neuropathic pain in cancer patients.
a. Celiac Plexus Block
The celiac plexus is a collection of nerves located near the abdomen that controls many of the internal organs, including the liver, pancreas, and gastrointestinal tract. A celiac plexus block involves injecting local anesthetic and/or steroids into the celiac plexus to relieve abdominal pain, particularly in patients with pancreatic cancer.
-
Indications: It is most commonly used for managing severe abdominal pain caused by pancreatic cancer or other abdominal cancers.
-
Benefits: The celiac plexus block can provide immediate and lasting pain relief, improving quality of life.
-
Outcome: Patients who undergo this procedure often report a significant reduction in pain, and in many cases, the relief can last for weeks or even months.
b. Neurolysis
In more severe cases, where a nerve block is not effective enough, neurolysis may be used to destroy the nerve causing pain. This can be done using chemicals, such as phenol or alcohol, or by using radiofrequency energy.
-
Indications: Neurolysis is often used for managing chronic pain caused by tumors compressing or infiltrating nerves.
-
Benefits: It can provide long-term relief by effectively cutting off the pain signals transmitted by damaged nerves.
-
Outcome: The success of neurolysis depends on the location of the nerve and the extent of tumor invasion. While the relief can be long-lasting, the procedure can cause permanent loss of sensation in the treated area.
4. Spinal Interventions
Cancer can spread to the spine, causing severe pain due to nerve compression, bone metastasis, or spinal instability. Interventional radiology offers several options for spinal pain management in cancer patients.
a. Vertebroplasty and Kyphoplasty
Both vertebroplasty and kyphoplasty are procedures used to stabilize and relieve pain caused by compression fractures in the spine, which may be due to cancer metastasis.
-
Procedure: In vertebroplasty, a cement-like material is injected into the vertebra to stabilize it and relieve pain. Kyphoplasty involves a balloon being inserted into the vertebra to restore its shape before injecting the cement.
-
Indications: These procedures are particularly useful for patients with metastatic cancer affecting the spine, including breast, prostate, or lung cancer.
-
Benefits: These minimally invasive procedures help restore stability to the spine, provide pain relief, and improve mobility.
-
Outcome: Vertebroplasty and kyphoplasty can significantly improve pain levels and reduce the need for pain medications.
b. Spinal Cord Stimulation (SCS)
For patients with intractable pain caused by cancer affecting the spine or nerves, spinal cord stimulation can be an option. In this procedure, a small device is implanted under the skin that sends electrical impulses to the spinal cord, interrupting the pain signals before they reach the brain.
-
Indications: Spinal cord stimulation is typically used for patients with neuropathic pain that cannot be controlled by medications alone.
-
Benefits: This technique can provide effective, long-term pain relief with minimal side effects.
-
Outcome: While spinal cord stimulation does not treat the underlying cancer, it can significantly reduce pain and improve function in patients with advanced cancer.
5. Biliary Drainage and Stenting
Biliary drainage and stenting are minimally invasive procedures used to manage blockages or narrowing in the bile ducts. The bile ducts transport bile, a fluid essential for digestion, from the liver to the intestines. When these ducts are obstructed due to conditions like gallstones, tumors, or scarring, it can lead to jaundice, pain, and serious complications like infections or liver damage.
Purpose of Biliary Drainage
Biliary drainage helps restore bile flow by either draining it externally or internally. It alleviates symptoms such as jaundice, itching, and abdominal pain and prevents complications like bile duct infections (cholangitis).
Procedure
Performed by an interventional radiologist, the process involves:
-
Imaging Guidance: Using ultrasound or fluoroscopy to visualize the bile ducts.
-
Catheter Insertion: A thin tube is inserted through the skin into the bile duct to drain bile externally (percutaneous biliary drainage) or internally.
-
Stenting: A stent (small tube) is placed in the duct to keep it open and ensure continuous bile flow.
Indications
-
Obstructive jaundice due to tumors (e.g., pancreatic or bile duct cancer).
-
Gallstones causing bile duct blockage.
-
Post-surgical strictures.
-
Infection management (cholangitis).
Benefits
Biliary stenting is less invasive than surgery, offers quick symptom relief, and improves quality of life for patients with conditions like advanced cancer.
Recovery and Care
Patients recover quickly, though some may experience mild pain or fever post-procedure. Regular follow-ups ensure the stent functions properly and prevents complications.
6. Embolization
Embolization is a technique that involves blocking the blood supply to a tumor, causing it to shrink and die. This procedure can be used to treat various types of cancer, including liver cancer, uterine fibroids, and some metastatic cancers.
-
Procedure: During embolization, small particles or coils are injected into the blood vessels supplying the tumor, blocking the flow of blood and oxygen to the tumor. This leads to tumor cell death.
-
Indications: Commonly used for liver cancer and metastases.
-
Benefits: It provides relief from both the tumor and the pain it causes, and it can sometimes shrink the tumor enough to make other treatments more effective.
-
Outcome: Embolization can provide lasting pain relief and reduce the size of the tumor, improving overall patient comfort.
Conclusion
Cancer-related pain is a multifaceted issue that requires a personalized approach to treatment. Interventional radiology has emerged as a key component in managing this pain, offering minimally invasive solutions that target the source of pain while preserving the patient's quality of life. Through techniques like tumor ablation, nerve blocks, spinal interventions, and embolization, interventional radiology plays an essential role in palliative care for cancer patients.
By working closely with interventional radiologists, oncologists, and palliative care teams, patients can benefit from advanced, targeted pain management techniques that provide meaningful relief without the need for major surgery. If you or a loved one is experiencing cancer-related pain, discussing these interventional options with your healthcare provider may open up new possibilities for relief and a better quality of life.
What's Your Reaction?







.jpg)
.jpg)

